Common Skin Issues
Acne
Acne is a disease that affects the oil-producing sebaceous glands in the skin. Sebaceous glands produce oil called sebum that begin to produce larger quantities of oil during puberty due to changing hormones. Acne occurs when the path of the sebum is blocked by dead skin cells. When sebum builds up around hair follicles, it becomes infected leading to the basic acne pimple. In some cases, the follicle can become so full that it bursts resulting in a large and painful lump under the skin known as an acne nodule. Acne nodules often leave scars when they heal which is why it is best to never squeeze or pop pimples on your own.
Contrary to popular belief, greasy foods and poor hygiene do not cause acne. Scubbing with harsh cleansers may actually worsen acne. If you suffer from moderate-severe acne, see a board-certified dermatologist for treatment to prevent inflaming the skin.
Common acne treatments include the following:
– Topical medications
– topical antibiotics
– chemical-peels
– Oral antibiotics
– Hormonal medications
– Contraceptives
– Pro-estrogen products
– Isotretinoin/Accutane for moderate-severe acne patients.
Isotretinoin gets a bad reputation from non-medical bloggers but has been on the market for over 40 years and is completely safe. In fact, it has the highest rate for providing a lifelong acne cure to people who suffer with severe acne.
Blistering Disorders
Blisters are caused by friction, trauma or internal conditions to the skin. They are formed when fluid accumulates between two layers of the skin. Diagnosis of a particular blistering disorder is usually done via biopsy in which a skin sample is taken from a blister’s edge for microscopic evaluation. Some autoimmune diseases produce blisters when antibodies attack the skin cells. Sometimes a test called immunoflourescence is performed to look for specific immune proteins that help distinguish one blistering disorders from another. Treatment for blistering disorders vary according to cause and severity.
Dark Spots
There are many potential causes of dark spots or hyperpigmentation. These can range from dreaded skin cancer melanomas to hormonal conditions like melasma or even inflammatory conditions such as acne. The easiest way to prevent all types of dark spots is to use a high-quality sunscreen that contains zinc oxide or titanium dioxide with a minimum SPF 30.
Melasma is an estrogen-derived form of hyperpigmentation affecting sun-exposed areas of the face. It is often called ‘the mask of pregnancy.’ Treatment for melasma often includes sun protection, prescription strength Vitamin A, low potency steroids, and prescription strength bleaching creams.
Acne-derived hyperpigmentation requires treatment of the underlying acne first and foremost to prevent new dark spots from forming. Chemical peels, laser resurfacing and bleaching creams may be recommended in more resistant cases.
Skin cancer melanomas or pigmented basal cells can also present themselves as dark spots. Dr. Claiborne uses dermoscopy, the latest technique in dermatology, to best identify whether a dark spot is potentially cancerous. If you suspect a dark spot may be cancerous, it is best to schedule an appointment immediately to have it looked at by an experienced board-certified dermatologist. Routine skin cancer screenings are also recommended if you know you have a history of skin cancer in your family.
Eczcema
Eczema (or dermatitis) describes a grouping of reaction-pattern of skin disorders with a variety of common characteristics. The acute disease is characterized by inflammation, redness, swelling, itching as well as some blistering, flaking and oozing.
Chronic dermatitis is identified by the thickened, leathery skin with excess ridges and darkened, dull appearance. When dermatitis becomes subacute, the intense reaction becomes milder and the blisters begin to heal.
Patients with a history of eczema must be careful to avoid dyes and fragrances, instead opting for gentle soaps and moisturizing creams and ‘free and clear’ detergents. Topical steroids are used to decrease itching and inflammation.
At MD Claiborne, our offices have phototherapy units – a non-immunosuppressive option for severe eczema in patients of all ages. In some cases, severe eczema can be treated with oral systemic medications such as methotrexate or cyclosporine, a hot new research topic as biologic drugs are evolving to modulate the immune system to prevent inflammatory diseases. The newest drug, Dupuixient, is a targeted biologic therapy for refractory atopic dermatitis patients. Dr. Cole Claiborne was involved in the clinical trials for this groundbreaking medication and can assess your suitability for this medication.
Herpes Simplex Virus
Herpes simplex virus (HSV-1 and HSV-2) causes outbreaks on the skin and mucous membranes. They are often referred to as cold sores. Herpes simplex virus lies dormant after initial infection and can become reactivated by exposure to ultraviolet light, emotional stress, surgery, trauma, or fluctuating hormone levels. The virus reproduces and travels down the nerve to the skin where it produces recurring infections.
While there is no cure for herpes, oral antiviral medications like famciclovir (Famvir), valacyclovir (Valtrex), and acyclovir (Zovirax) may be given to treat recurrent episodes or prevent recurring outbreaks. Some topical products such as antiviral creams, penciclovir (Denavir), and numerous over-the-counter topical remedies can also be used.
The best prevention against herpes simplex virus is to reduce the risk of exposure by having open discussions with potential sexual partners. Condoms should be used, although they are not always effective at preventing the spread of herpes. Someone with an outbreak of herpes simplex virus should avoid sex until all lesions and blisters have crusted over.
Hives
Hives, also known as urticaria, are raised red bumps on the skin caused by the release of histamine and other inflammatory substances usually in response to an irritant or allergen. The most common triggers include upper respiratory tract infections, reactions to prescription drugs, and even food allergens. Sensations with these lesions include itching, stinging, prickling and pain.
Urticaria lasting less than 6 weeks is classified as acute urticaria while urticaria lasting over 6 weeks is classified as being chronic. Chronic urticaria is more common in middle-aged females while acute urticaria is more common in children. Chronic urticaria requires systemic workup by a board-certified dermatologist for identifying potential causes.
The first-line therapy to treat urticaria consists of various antihistamines. Some alternative therapies can include oral steroids, phototherapy, leukotriene inhibitors and cyclosporine. A novel injectable biologic known as Xolair (omalizumab) was approved by the FDA in March 2014 for treatment of chronic urticaria in patients over the age of 12 who did not respond to antihistamine treatment.
Hyperhydrosis
Hyperhydrosis is the medical name for excessive chronic sweating disorder that affects nearly 8.8% of the population. Hyperhydrosis causes one to sweat disproportionately to certain stimuli and can be damaging to a person’s self-esteem. People with hyperhydrosis sweat 4 to 5 times more than the average person which can result in embarrassing sweat stains and discomfort that causes the person to refrain from activities where they are prone to sweat and avoid certain social or business situations where their condition may flare up.
In some cases, hyperhydrosis is a secondary symptom of another medical situation such as diabetes, menopause or cancers. It can also be a side-effect of some medications like antidepressants. It is important to consult a board-certified dermatologist in order to identify whether you have primary or secondary hyperhydrosis and discuss the best treatment options. Common treatment options include prescription grade antiperspirants, botox injections, laser treatments, and in extreme cases surgeries to remove excess sweat glands.
Keloids
Keloids are firm, fibrous tissue nodules typically found in areas of previous skin trauma such as burns or scars. They can be single or scattered across an area of the skin and may be itchy or painful following the inciting trigger. Keloids can be very disfiguring and restrict normal motion causing significant discomfort. Keloids are most common in African-Americans and people of Mediterranean descent but may appear in people of any ethnicity.
Keloids can be quite difficult to treat. Excision of keloids are only performed if there is a post-procedure plan to prevent recurrence. Injectable steroids are often used to cause atrophy of the keloids so they are softer and less raised. On occasion, radiation therapy or chemotherapeutics such as 5-fluorouracil are used.
Psoriasis
Psoriasis is a non-contagious common skin condition that causes rapid skin cell reproduction that results in red, dry patches of thickened or scaly skin commonly affecting the elbows, knees, back and scalp.
Psoriasis symptoms can range from mild to severe where the entire body is virtually covered in thick red scaly skin. Psoriasis is a chronic, non-curable skin condition that can periodically improve and worsen. Some people notice psoriasis conditions worsen with cold dry weather and improve with warmer months and increased sun exposure, In some cases, people can even experience psoriasis remission for years.
Psoriasis affects all races and sexes worldwide and currently affects about 8 million people in the USA. It is an autoimmune condition that is often diagnosed in young adulthood.
MD Claiborne Dermatology is one of the few practices to offer full-body narrow band ultraviolet B (nbUVB) phototherapy treatment as a non-immunosuppressive treatment option for plaque psoriasis. For moderate to severe psoriasis, we use highly effective advanced biologics therapies to calm the overactive immune system.
There are three main types of biologics available:
1. Anti-TNFs (Humira/Enbrel/Remicade/Cimzia)
2. Anti-IL17s (Cosentyx/Taltz/Siliq)
3. Anti-IL23s (Skyrizi/Tremfya)
Drs. Martin and Cole Claiborne specialize in the treatment of psoriasis and have an ongoing clinical trial for psoriasis sponsored by U Penn and the National Psoriasis Foundation.
Rashes
While the word ‘rash’ does not have an exact meaning or refer to a specific disease or kind of disorder, it is a general term that refers to the outbreak of bumps on the body that change the way one’s skin looks and feels. Rashes can be localized to one area or be widespread across the body and can refer to many different skin conditions.
Rashes refer to an inflamed area of irritated skin that is characterized by redness, itching, swelling and various types of skin lesions such as macules, papules, nodules, plaques, pustules, vesicles, and wheals. In some cases, the area of affected skin is dry and sensitive and warm to the touch. In other cases the skin can crack and flake. Most people will experience some type of rash during their lifetime. Most rashes are not serious, but in rare instances, a rash can indicate a life-threatening condition. It is important to see a board-certified dermatologist at the onset of a rash to receive accurate diagnosis and treatment.
The four main categories of rashes are as follows:
1. Scaly patches of skin not caused by infection.
2. Scaly patches of skin caused by fungal or bacterial infection.
3. Red itchy bumps or patches across the body.
4. Allergic reaction such as hives.

Rosacea is a skin disease that causes redness and swelling of the face. As the disease progresses, it can cause tiny pimples to appear on and around the reddened area. Rosacea develops over an extended period of time. It may first seem like one may have a tendency to blush easily, have a ruddy complexion or have an extreme sensitivity to cosmetics. Approximately half of rosacea patients experience burning and grittiness of the eyes also known as conjunctivitis, which should be treated immediately. In advanced cases, rosacea can be characterized by an enlarged red nose and puffy cheeks.
Treatment options for rosacea include topical medications in milder cases or oral antibiotics for moderate-severe cases. In certain cases, rosacea can be treated with a small electric needle, state-of-the-art laser therapy or minor surgery to close off dilated blood vessels. While the cause of rosacea is unknown, certain factors can irritate the condition such as too much alcohol, prolonged sun exposure, temperature extremes, irritating cosmetics/detergents, and too much massaging of the face.
Shingles
Shingles, or Herpes Zoster, is a painful rash that can affect anyone who has had chickenpox. When someone has had chickenpox, the varicella-zoster virus that triggers the chickenpox, remains in the body, usually in a dormant state. Shingles results when something triggers the dormant virus to wake-up, resulting in a blistering rash that covers the body. Most people who get shingles are aged 60 and above.
Shingles is not as contagious as chickenpox, but it can spread if someone comes in contact with fluid from a broken shingles blister. The shingles blisters eventually scab over and heal within two to four weeks, though there can be losting complications such as post-herpetic neuralgia (PHN) that affects the nerves, herpes zoster ophthalmicus that affects vision, or other skin infections.
Early detection of shingles can lessen the risks of complications. A board-certified dermatologist will often prescribe antiviral medications to lessen the pain and severity of the shingles outbreak in addition to recommending pain relievers and wet cloths to alleviate pain and itching. In extreme cases, a nerve block may be injected to help numb the area.
For adults aged 60 and older, the FDA recommends getting the shingles vaccine to prevent shingles outbreaks. Studies show a 50% decrease in risk of developing shingles in people who receive the shingles vaccine. Before getting the shingles vaccine, talk to your doctor to review current medications and medical history.
Skin Allergies
Skin allergy refers to a type of allergic contact dermatitis caused when a person’s skin comes into contact with a substance that induces an inflammatory reaction. There are two basic types of contact dermatitis: Irritant Contact Dermatitis (ICD) and Allergic Contact Dermatitis (ACD).
Irritant Contact Dermatitis (ICD) refers to a non-specific inflammatory condition that develops after skin is exposed to substances that are physically, chemically or mechanically traumatizing. Symptoms are usually confined to the area of contact, recur with additional irritant exposure and may be difficult to distinguish from allergic contact dermatitis.
Allergic Contact Dermatitis (ACD) is a form of contact dermatitis that occurs from a person’s immune response to contact allergens such as fragrances, preservatives, metals, etc. ACD. can develop within hours or days and may take weeks to heal. To identify which substance(s) a person may be allergic to, Dr. Claiborne uses the T.R.U.E. Test to test 35 different allergens. This test is referred to as a ‘patch test’ which is different than the ‘prick test’ or ‘scratch test’ that requires breaking the skin to introduce the irritant. The T.R.U.E. Test is a topical test where the irritants are introduced topically. The T.R.U.E. Test only tests for skin irritants and is not used to identify allergens associated with anaphylaxis.
Skin Cancer
Skin Cancer is the most common of all cancers. Over one million Americans develop skin cancer every year. Overexposure to sunlight and tanning is the main cause of skin cancer, especially when it results in the blistering of skin. Other less common factors can include repeated medical and industrial x-ray exposure, scarring from diseases and burns, occupational exposure to harsh compounds such as coal and arsenic, or a family history of skin cancer. Fair-skinned people who sunburn easily are at particularly high risk for skin cancer and should always take precaution by wearing sunscreen with an SPF 30 or higher daily.
Basal Cell Carcinomas are a form of skin cancer most often found in fair-skinned people. It rarely is found in African American patients. Basal Cell Carcinomas are characterized by their fleshy nodule-like appearance often on the head, neck and hands. These tumors do not grow quickly. Left untreated, they will bleed, crust over, heal and then begin the cycle again.
Squamous Cell Carcinoma is characterized by red scaly patches or bumps and is the second most common type of skin cancer. It is usually found on the rim of the ear, the face, the lips and the mouth and is more likely to affect fair-skinned people than darker skinned people. This type of cancer can metastasize, but if caught early and treated by a board-certified dermatologist, there is a 95% rate of cure.
Malignant Melanoma is the most deadly form of all skin cancers and is characterized by asymmetric spots or bumps on the skin with irregular borders and non-uniform pigmentation of brown or black coloration. It is important to routinely check moles for development of these features especially if you have a family history of skin cancer. Any growing or changing mole should be evaluated by Dr. Claiborne immediately.
Treatment options for skin cancer depends on the type of skin cancer, size of the skin cancer and location of the skin cancer on the body. Potential treatments include excision with stitches, superficial radiation, Mohs micrographic surgery, and/or topical chemotherapy.
Vitiligo
Vitiligo is causes skin pigmentation to lessen and lighten in patches in a localized area or across the entire body. Vitiligo is triggered when the melanocyte cells that give skin its pigment die, causing skin to fade. It is unknown what causes these cells to die. Some medical experts consider vitiligo to be a type of autoimmune disease. In most cases skin pigment may return with time, but for some, the color loss can be permanent if not treated.
Vitiligo affects people of all races. It often begins between ages 20 and 40. If you suspect you may have vitiligo or have been diagnosed with vitiligo and require treatment, a board-certified dermatologist can offer a range of treatment options from ultraviolet light therapy, topical treatments, skin grafts or depigmentation treatments.
Warts
Warts are non-cancerous skin growths caused by a viral infection in the top layer of the skin and mucus membranes. Viruses that cause warts belong to a family called human papillomavirus (HPV)). Warts are usually skin colored and feel rough to the touch, but they can also be dark, flat or smooth.
There are several types of warts: common warts around nails on the fingers and toes, foot warts also called plantar warts on the bottoms or soles of the feet, and flat warts that are flat and sooth. Flat warts can grow in great numbers at one time and affect any part of the body.
Warts should be treated to avoid spreading to other body parts or other people. They are most commonly treated with salicylic acid, cryotherapy (freezing) or electrodesiccation (burning). Depending on the depth of the wart, several treatments may be required. For warts that are especially stubborn to treatment, bleomycin injections can be used.
Hair/Nail Disorders

Hair Disorders
Hair grows on human skin in various textures, colors and densities. The structure that each hair grows from is called the follicle. Muscles, oil glands and nerves extend from the follicle into the dermis layer of the skin. Throughout life, the skin is constantly shedding dead skin cells and growing new ones. Inside the hair follicles, sebum oil carries the dead cells to the surface of the skin. Various factors can interfere with the cycle of renewal and disposal causing a number of hair disorders.
Folliculitis is infection and inflammation of the hair follicle. The condition may only be superficial and affect the surface of the skin, or it may extend deep within the follicle. The most common cause of folliculitis is bacterial Staphyloccus aureus. Hair follicles become red and irritated resulting in pus-filled lesions. Folliculitis can clear up by itself in a matter of weeks or, when persistent, requires treatment by a board-certified dermatologist.
Alopecia. is the medical term for baldness. It is an autoimmune disease that leads to hair loss anywhere on one’s body including eyelashes and eyebrows. Alopecia can affect men, women and children, causing the person’s immune system to attack the hair follicle and the hair to stop growing and fall out. Alopecia results in overall thinning of scalp hair rather than complete balding. Alopecia areata and androgenetic alopecia are types of temporary hair loss that does not result from damaged follicles. Scarring alopecia is permanent hair loss that results from damaged follicles. Dr. Claiborne may opt to do a scalp biopsy to determine whether the cause of your alopecia is due to a scarring or non-scarring form of alopecia.
Treatments for alopecia can include topical treatments, oral treatments or injectable treatments depending on the cause and severity of your hair disorder.

Nail Disorders
Nails can be affected by a number of disorders. The most common nail disorder is a fungal infection that causes abnormal nail growth, discoloration, nail separation and nail thickening. Nail infections are more common in immunosuppressed patients and are often paired with fungal infections of the feet. In addition to fungal infections, other nail disorders can be related to infections and internal diseases, birth defects and growth problems, drug use and more.
Pediatric Dermatology

Drs. Martin and Cole Claiborne have extensive training in treating pediatric conditions of the skin. During his residency, Dr. Cole Claliborne trained at Children’s Hospital Dermatology Clinic and is adept at treating infants to adolescents. He maintains an active membership with the Society for Pediatric Dermatology.
The most common pediatric skin condition is eczema. Pediatric patients with eczema have sensitive skin types and parents should make a significant effort to minimize their exposure to dyes and fragrances in soaps and detergents. Other common conditions in children and adolescents include acne, fungal infections, molluscum contagiosum and vascular growths. Early intervention is needed to prevent worsening of skin disorders in younger patients.
Fungal Infections

Skin Fungus
Fungal infections of the skin are given the general name ‘tinea.’ Superficial fungal infections affect the top layers of the skin including the mucous membrane, hair and nails. Common examples of superficial fungal infections are athlete’s foot, jock itch, ringworm and candida. Deep fungal infections are of much more concern as they can spread to the blood and internal organs if left untreated. Yeast and fungal infections are typically treated with topical or oral antifungal medications. Antibiotics may lead to fungal infections despite killing bacteria. Fungus tend to grow in warm, moist areas of the body such as the armpit, groin region and feet.
Blood Vessel Disorders
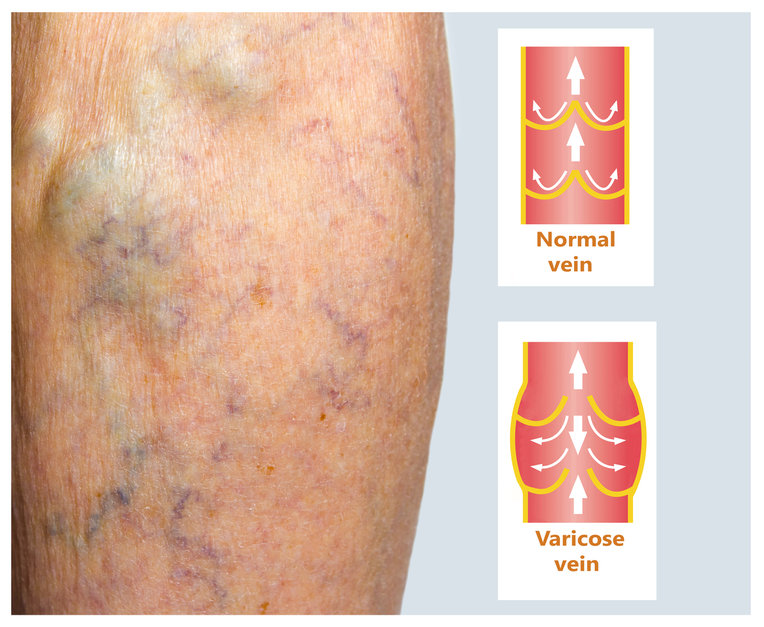
The blood supply in the skin is delivered by an interconnecting network of small arteries and veins. In the embryo, certain cells are responsible for stimulating blood vessel development. Simple tubelike blood vessels form first and then develop fully through the process of angiogenesis. The vasculature blood vessel network is the first organ to begin developing in embryo and continues until adulthood. Some blood vessel disorders are the result of the overproduction of blood vessel cells including angiomas (spider veins), varicose veins and telangectasias. Depending on the type and size of your blood vessels, treatments include laser therapy and injectable sclerotherapy. Drs. Martin and Cole Claiborne also treat infantile hemangiomas which are vascular malformations that occur during pregnancy and result in port-wine stains on the infant at birth.
Surgical Dermatology
MD Dermatology offers surgical dermatology procedures as treatment options for skin cancers, lipomas, abnormal moles and cysts. While in most circumstances, surgery is used as a last resort, Drs. Martin and Cole Claiborne are skilled and experienced surgeons.
SKIN CANCER SURGERIES
1. Squamous Cell Carcinoma
Squamous Cell Carcinomas (SCC) can be rough bumps, flat red patches, dome shaped bumps or open sores that do not heal. They often result from excess sun exposure and, when left untreated, can spread to other parts of the body. To diagnose SCC, a board-certified dermatologist will perform a biopsy using local anesthesia and examine the sample under a microscope. To treat SCC, surgical excision is often necessary. Most excisions are done under local anesthetic during an office visit and may require stitches. Mohs’ surgery is another surgical option that is performed in a medical office under local anesthesia. The patient remains awake as the affected skin cells are removed and examined under a microscope. The surgeon will continue to scrape away tissue until all traces of cancerous cells are removed.
2. Basal Cell Carcinoma
Basal Cell Carcinomas (BCC) are dome-shaped growths with visible blood vessels. They can appear shiny and pink in color or white and yellow. Most BCCs develop on areas that have been affected by extended sun exposure over time. When detected early, BCC can be treated effectively with biopsy and excision or Mohs micrographic surgery.
3. Malignant Melanoma
Malignant Melanoma is the most serious form of skin cancer that produces dark colored moles with irregular borders. Melanomas are greater than 6mm in diameter, asymetrical and will evolve in shape, size and color. Early detection is key when dealing with Malignant Melanoma, especially when one has had extensive sunexposure or repetitive sunburns, or has family history of melanoma. The most common treatment forms for melanomas are surgical excision, Mohs Micrographic Surgery, chemotherapy and radiation. Your dermatologist will discuss treatment options with you.
